Stereotactic EEG (SEEG)
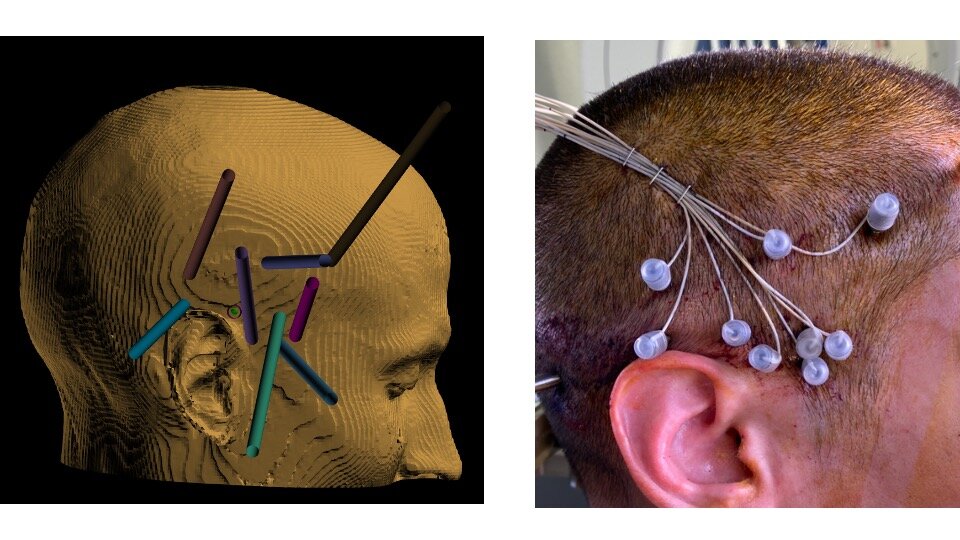
Stereotactic EEG. 3D software (left panel) is used to plan trajectories to the targets in the brain. A surgical robot helps me place them in a minimally invasive manner with sub-millimeter accuracy, requiring only tiny incisions in the skin (right panel).
What is SEEG?
Stereotactic EEG (SEEG, or stereoencephalography) is a minimally invasive technique for studying seizure networks. I use it to help understand where epileptic seizures arise. In an SEEG procedure, millimeter-thin wires are introduced precisely into the brain using 3D planning software and a surgical robot (see photo below). SEEG has numerous advantages over other methods for studying seizure networks in the brain.

Who is this procedure for?
SEEG is used for patients with medication-resistant epilepsy to understand where in the brain seizures are arising. It is an important step that helps me select between different surgical therapies for epilepsy patients, including craniotomy, laser ablation, deep brain stimulation, and responsive neurostimulation.
The goal of SEEG is to identify a patient's seizure onset zone with millimeter precision. SEEG electrodes are much more effective than traditional skin/scalp electrodes for studying seizures because they can be much closer to the source of the seizures.
What can a patient expect from the procedure?
Before surgery, I will discuss your case with your epilepsy doctor, and together we will decide on the parts of the brain that we think might be involved in your seizures. I will order an MRI and CT scan of your brain to help plan the placement of the wires.
You will be admitted to the hospital on the day of surgery. The procedure is performed under general anesthesia. During surgery, I will insert several thin wires into your brain using robotic guidance. Each wire passes through a tiny skin incision and a 2 millimeter hole drilled in the skull. These holes are not visible after the operation, and each incision will ultimately be closed with a single stitch. I will wrap a bandage around your head and then wake you up from anesthesia.
The rest of your hospital stay will be very similar to the traditional epilepsy monitoring unit admission that you had before, except this time the electrodes will be inside your brain rather than on your skin. We will wait for you to have seizures, and we may need to temporarily reduce or stop some of your anti-seizure medicines. I prefer to record several seizures so that we can be confident about where they are starting. On average, this takes 7-10 days.
Once we have enough information about your seizures, I will remove the wires under sedation in the operating room. You will be able to go home later that day or the following morning. I will then meet with you in my clinic to discuss what we found and what the options are for treating your epilepsy with surgery.
What are the benefits and risks?
The benefit of SEEG is that we have a good chance of finding the starting zone for your seizures (>95% in large clinical studies). Localizing your seizures means that we can select the best surgical therapy for you. Some surgical therapies can even be curative.
The main risk of SEEG is bleeding in the brain. This risk is low (about 1% in large studies), in part because the robot and 3D software help us avoid blood vessels and the wires themselves are not very stiff. SEEG has a better safety and tolerability profile than traditional forms of invasive monitoring for epilepsy.
I have a particular interest and specialized training in caring for patients with epilepsy, and I am the director of epilepsy surgery at Swedish Medical Center, a level 4 epilepsy center.
Below is additional information on stereotactic EEG (SEEG). If you live near Denver and have epilepsy that has not responded to medications, please consider meeting me in consultation to learn about treatment options.